Resorbable Poly-(D,L)-Lactide Anchorage of Nanoparticulate Mineralized Collagen Materials Maximizes In Vivo Skull Regeneration
Resorbable Poly-(D,L)-Lactide Anchorage of Nanoparticulate Mineralized Collagen Materials Maximizes In Vivo Skull Regeneration
Bedar, M.; Ren, X.; Chen, W.; Kang, Y.; Moghadam, S.; Huang, K. X.; Shariati, K.; Harley, B. A. C.; Lee, J. C.
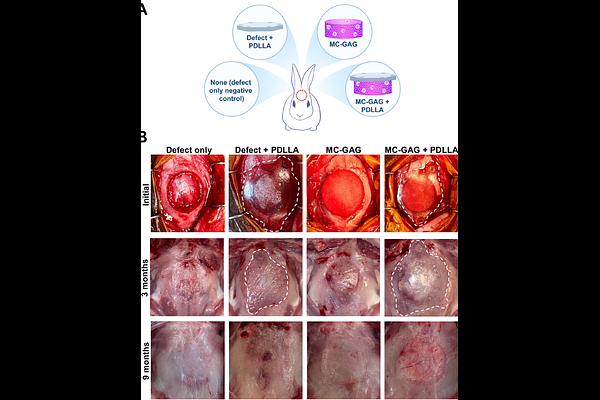
AbstractBackground A clinical demand exists for bone biomaterials that mirror tissue-specific extracellular matrix (ECM) properties and regulate progenitor cell fate. Nanoparticulate mineralized collagen glycosaminoglycan (MC-GAG) scaffolds have demonstrated to promote skull regeneration in vivo without addition of growth factors or exogenous progenitor cells, offering a materials-only solution for cranial defect reconstructions. Further enhancement of the safety and regenerative potential of MC-GAG is however necessary for clinical translation. Here, we investigated the regenerative effect of MC-GAG scaffold fixation with a resorbable poly(D,L-lactide) (PDLLA) implant for cerebral protection. Methods Fourteen-millimeter cranial defects were created in New Zealand white rabbits, divided into four groups: 1) defect only, 2) defect with PDLLA, 3) MC-GAG, and 4) MC-GAG with PDLLA. Initial bone healing assessment was conducted at 3 and 9 months using microcomputed tomography (microCT), histology, reference point indentation, and scanning electron microscopy. Long-term effects were evaluated through in vivo microCT imaging at 3, 6, and 9 months, with biomechanical testing of explanted skulls at 9 months. Results At 3 months, MC-GAG significantly enhanced mineralization compared to empty and PDLLA-treated defects, with even greater mineralization observed for MC-GAG-PDLLA. Histologically, MC-GAG demonstrated trabecular mineralization, while MC-GAG-PDLLA had a structural organization resembling native bone. Biomechanical assessment showed enhanced toughness and stiffness for both MC-GAG and MC-GAG-PDLLA. At 6 months, MC-GAG-PDLLA displayed the highest bone mass, and at 9 months, both MC-GAG-containing scaffolds demonstrated superior bone regeneration compared to controls. By 9 months, PDLLA implants were completely resorbed and MC-GAG-PDLLA exhibited mechanical properties surpassing those of all other groups. Conclusions Fixation of MC-GAG scaffolds with PDLLA implants improved mineralization and bone regeneration compared to either material alone for cranial defect reconstruction.