Tissue resident memory T cells populate the human uveal tract
Tissue resident memory T cells populate the human uveal tract
Foers, A. D.; Reekie, I. R.; Wickramasinghe, L.; Ward, A.; Buckley, T. M.; Attar, M.; Aguilar-Munoa, S.; Pilapil, Q.; Abdalla Elsayed, M. E.; Pledger, S.; Bhalla, A.; Hedley, R.; Hill, S.; Windell, D.; Barton, K.; Masood, I.; Lim, K. S.; Coles, M. C.; Sherlock, J. P.; Dick, A. D.; Coupland, S. E.; Sansom, S. N.; Copland, D. A.; Buckley, C. D.; Sharma, S. M.; ORBIT Consortium,
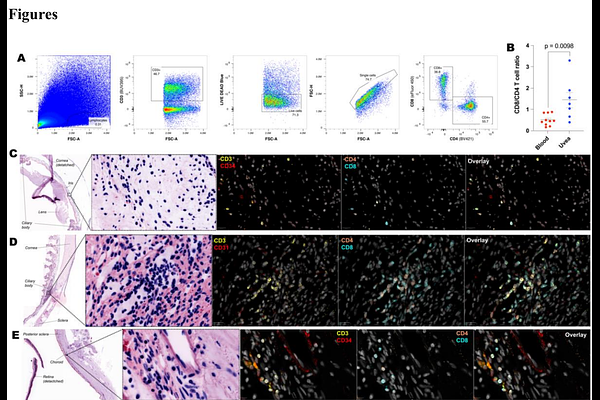
AbstractThe current concept is that the eye is an immune privileged site endowed with innate immune regulatory networks to maintain organ function. We now have evidence that resident T cells occupy intraocular tissues. In immune-mediated inflammatory diseases, such as psoriasis and rheumatoid arthritis, tissue resident T cells trigger disease flares in the skin and joints. This suggests resident T cells in the uvea may have similar functions in non-infectious immune-mediated uveitis, a collective term for autoinflammatory and autoimmune diseases of the uveal tract causing intraocular inflammation. Here, we demonstrate by spectral cytometry and immunofluorescence imaging that non-inflamed uveal tissue contains multiple T cell subtypes including CD8+ CD103+ tissue resident memory T (TRM) cells. Using single cell RNA & T cell receptor (TCR) sequencing to profile aqueous humour cells from donors with acute, active uveitis, we identify clonally expanded T cells which are enriched for TRM -associated genes. We further show that in donors with active uveitis, CD8+ CD103+ T cells persist within tissue in the uveal tract. Using bulk RNA sequencing and weighted gene co-expression network analysis (WGCNA) we show that quiescent iris tissue from donors with a history of uveitis are enriched for genes associated with T cell activation and antigen presentation. Finally, we demonstrate that TRM cells persist in the anterior uvea in mice following resolution of experimental autoimmune uveoretinitis (EAU). Our results show that the human eye contains T cells both in health and during active inflammation. Our findings challenge the dogma that the eye is devoid of lymphocytes and supports the concept of resident T cell involvement in the pathogenesis of non-infectious immune-mediated uveitis and as promising targets for therapy.