Prevalence, Production and the Role of Staphylococcus aureus Superantigens in Cystic Fibrosis Lung Disease.
Prevalence, Production and the Role of Staphylococcus aureus Superantigens in Cystic Fibrosis Lung Disease.
Sun, Y.; Hu, B.; Chhabra, S.; Tolentino, J.; Suzuki, N.; Natarajan, J.; Harris, Z.; Stanley, G.; Bianco, C.; Planet, P. J.; Sherchand, S. P.; Adhikari, R.; Aman, J.; Zhang, X.; Koff, J. L.; Rajagopalan, G.
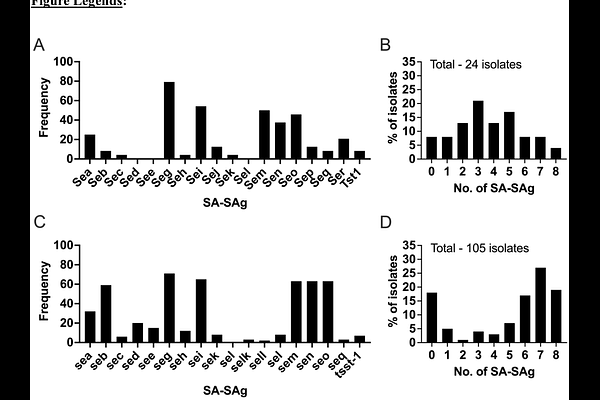
AbstractStaphylococcus aureus (SA), the most common cystic fibrosis (CF) lung pathogen, is uniquely capable of producing superantigen (SAg) exotoxins, which are the most potent activators of the immune system. Although the proinflammatory roles of SA-SAgs is well-established, their role in the immunopathogenesis of CF lung disease is unexplored. Herein, we demonstrate that 60-80% of pediatric and adult CF SA isolates carried at least one SA-SAg gene, with the former harboring potent SA-SAgs (Staphylococcal enterotoxin A and B) more frequently (30-60%). Biofilms of clinical SA isolates readily produced biologically active SA-SAgs in artificial sputum medium and purified SA-SAgs retained their bioactivity in human CF sputum in vitro. Repeated intratracheal challenge with purified SA-SAgs induced a robust pulmonary inflammatory response in CF mouse models ({beta}ENAC and CFGC transgenic mice) expressing HLA-DR3 in a dose-dependent manner, with the low dose favoring a type 2 eosinophilic lung inflammatory response, and a high dose eliciting a type 1 inflammatory response with neutrophilic lung inflammation and higher mortality. In vivo neutralization of IFN-{gamma} also promoted SA-SAg-driven type 2 inflammation. Intratracheal infection with sub-lethal dose of a clinical SA isolate producing SEB, but not the SEB-deficient mutant isogenic SA strain, also elicited an eosinophilic inflammatory response.