Mgl2+ cDC2s coordinate fungal allergic airway type 2, but not type 17, inflammation.
Mgl2+ cDC2s coordinate fungal allergic airway type 2, but not type 17, inflammation.
Cook, P. C.; Brown, S. L.; Houlder, E. L.; Baker, S.; Svedberg, F. R.; Howell, G.; Bertuzzi, M.; Boon, L.; Konkel, J. E.; Allen, J. E.; MacDonald, A. S.
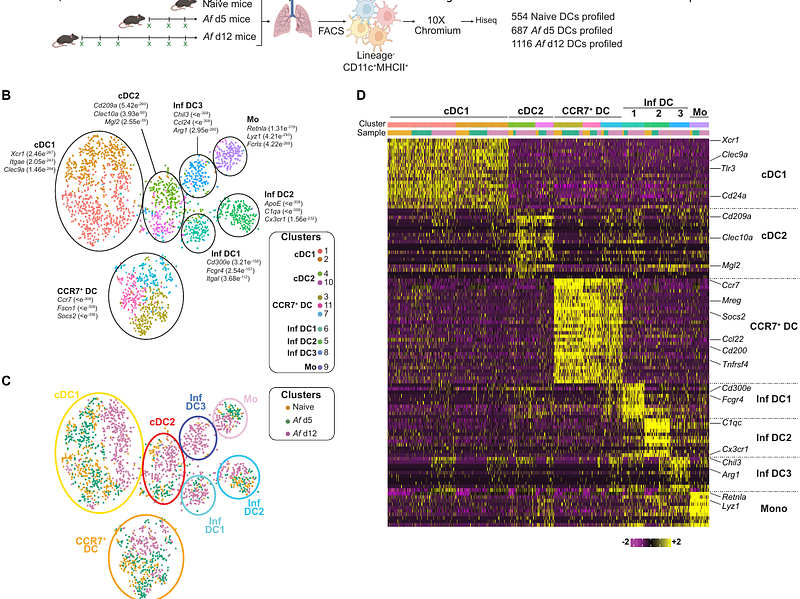
AbstractFungal spores are abundant in the environment and a major cause of asthma. Originally characterised as a type 2 inflammatory disease, allergic airway inflammation that underpins asthma can also involve type 17 inflammation, which can exacerbate disease causing failure of treatments tailored to inhibit type 2 factors. However, the mechanisms that determine the host response to fungi, which can trigger both type 2 and type 17 inflammation in allergic airway disease, remain unclear. We found that CD11c+ DCs and CD4+ T cells are essential for development of both type 2 and type 17 airway inflammation in mice when repeatedly exposed to inhaled spores. Single cell RNA-sequencing enabled the development of multi-parameter cytometry that identified allergic inflammation dramatically altered the proportion of numerous DC clusters in the lung, but that only two of these (Mgl2+ cDC2s and CCR7+ DCs) migrated to the dLNs. Targeted removal of several DC subsets revealed that only Mgl2+ cDC2 depletion dramatically reduced type 2, but not type 17, anti-fungal allergic airway inflammation. These data highlight distinct DC subsets are potential therapeutic targets for the treatment of pulmonary fungal disease.