Targeted Irradiation and STAT3 Inhibition Reprogram the AML Microenvironment and Extend Survival: Toward Translational Immunoradiotherapy
Targeted Irradiation and STAT3 Inhibition Reprogram the AML Microenvironment and Extend Survival: Toward Translational Immunoradiotherapy
Sargur Madabushi, S.; Brooks, J.; Zuro, D.; Yu-Lin, S.; Kaniowski, D.; Ghimire, H.; Eun Lim, J.; Abdelhamid, A. M. H.; Ya-Huei, K.; Marcucci, G.; Wong, J.; Al Malki, M.; Stein, A.; Kortylewski, M.; Hui, S.
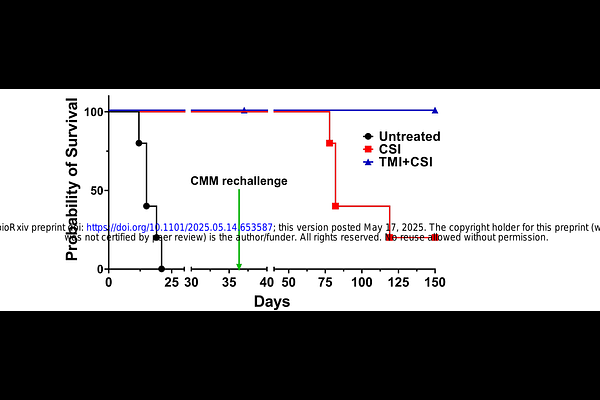
AbstractPurpose: Despite advances in acute myeloid leukemia (AML) therapy, relapses remain challenging. While AML is radiation-sensitive, total body irradiation (TBI) causes organ toxicities and activates tolerogenic/proangiogenic STAT3 signaling. CSI-2, a myeloid cell-targeted STAT3 inhibitor, promotes anti-leukemic immune responses but has limited efficacy against high disease burden. We investigated whether image-guided targeted marrow irradiation (TMI), which focuses radiation on leukemia sites while sparing critical organs, could synergize with CSI-2 to improve leukemia clearance and establish durable immunity. Methods: Mice were intravenously engrafted with CMM-AML cells reaching 20-30% in bone marrow (BM) infiltration (moderate-to-high disease burden) before receiving IV-injections of CSI-2 (5mg/kg) with or without TMI. Fluorescently-labeled CSI-2 biodistribution was assessed using flow cytometry and quantitative multiphoton microscopy. Survival was monitored for 3-4 months before evaluating BM composition using flow cytometry and immunohistochemistry. Results: TMI significantly improved vascular permeability and scavenger receptor/TLR9-dependent uptake of CSI-2 by AML cells and leukemia-associated myeloid cells. Combined TMI/CSI-2 treatment more effectively reduced high leukemia burden than CSI-2 alone, achieving >80% survival at 120 days with increased CD8+ cytotoxic and CD4+ helper T cell infiltration. TMI/CSI-2-treated mice were protected from AML rechallenge suggesting that they developed protective immune memory. In an aggressive MLL-AF9 AML model, TMI/CSI-2 combination significantly extended survival compared to either monotherapy. Conclusion: TMI/CSI-2 strategy represents a novel organ-sparing immunoradiotherapy that synergistically enhances leukemia clearance while promoting long-term protective immunity. These findings warrant further investigation of this strategy for high-burden or relapsed AML and provide the foundation for clinical translation.